Treatments
At Vascular & Vein Institute, our priority is to prevent amputation with our innovative treatments.
Invasive Procedures for PAD
Lower Extremities Angiogram
Lower Extremities Balloon Angioplasty
Lower Extremities Angiogram: Iodine vs. CO2
An angiogram of the lower extremities is an important imaging test that helps doctors evaluate blood flow in the legs. Traditionally, this procedure uses iodine-based contrast, but carbon dioxide (CO2) has emerged as a valuable alternative in certain cases. Let’s explore both options and what you can expect from this procedure.
Why is this test important?
An angiogram allows us to:
- Detect blockages or narrowing in your leg arteries
- Evaluate blood flow to your feet and toes
- Guide treatment decisions for conditions like peripheral artery disease
Early detection and treatment of circulation problems in your legs can help prevent serious complications and improve your quality of life.
Iodine-based Angiogram
This is the traditional method, using a liquid contrast agent containing iodine.
Benefits:
- Provides high-quality images
- Widely available and familiar to most doctors
Considerations:
- It may not be suitable for patients with kidney problems or iodine allergies.
- It can cause rare but serious allergic reactions
CO2 Angiogram
This newer method uses carbon dioxide gas as the contrast agent.
Benefits:
- Safe for patients with kidney problems or contrast allergies
- No risk of allergic reactions
- Rapidly cleared from the body through breathing
Considerations:
- Image quality may be slightly lower than iodine contrast in some cases
- Not suitable for imaging above the diaphragm
What to expect during the procedure
- You’ll lie on an examination table.
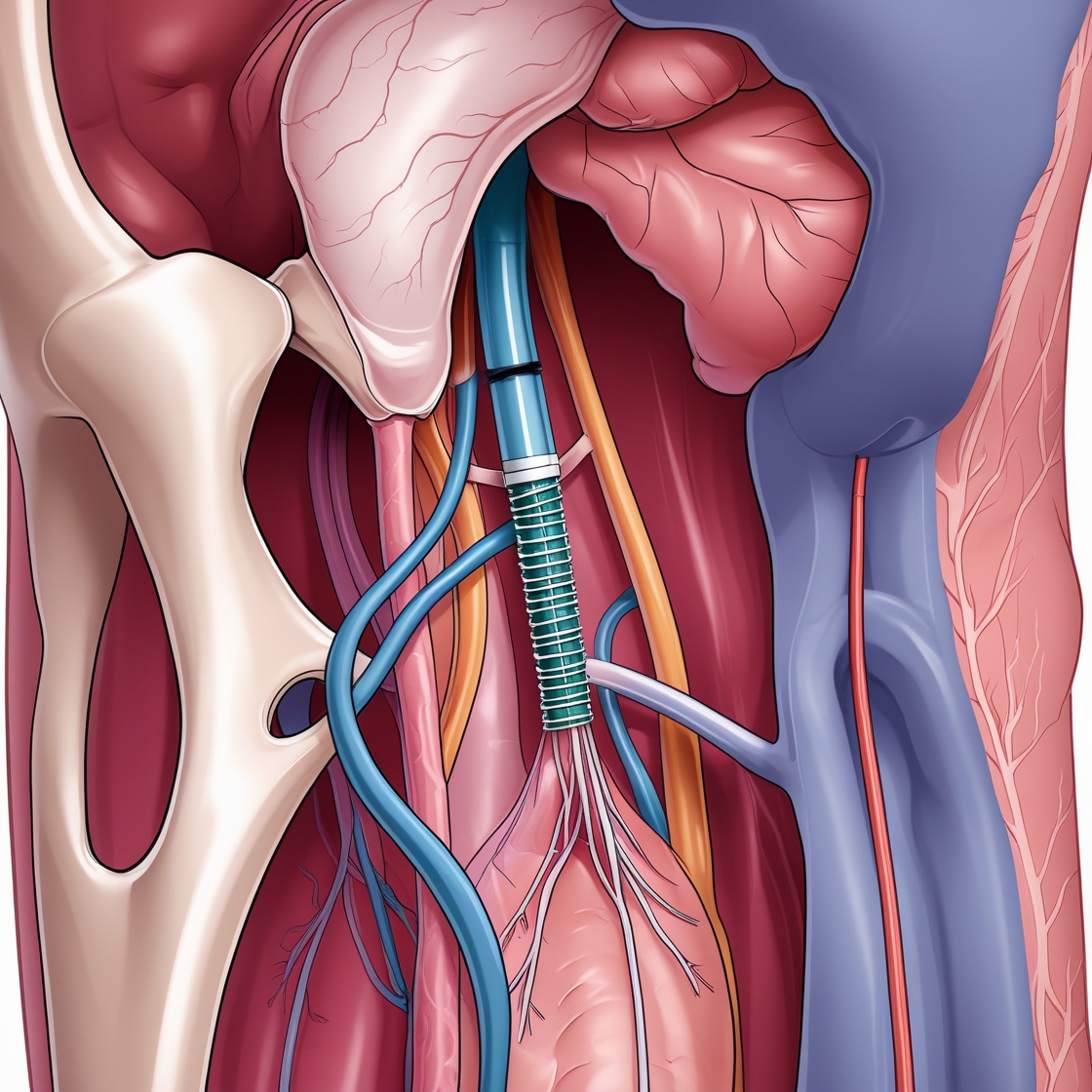
- A small catheter will be inserted into an artery, usually in your groin.
- The contrast (iodine or CO2) will be injected through the catheter.
- X-ray images will be taken as the contrast moves through your blood vessels.
- The procedure typically takes 30 to 90 minutes.
Preparation and aftercare
- You may be asked to fast for several hours before the procedure.
- Inform your doctor of all medications you’re taking.
- After the procedure, you’ll need to lie flat for a few hours to prevent bleeding at the catheter site.
- Most patients can go home the same day but should avoid strenuous activity for 24 hours.
How it benefits your health
An angiogram of the lower extremities helps us:
- Accurately diagnose circulation problems in your legs
- Plan the most effective treatment for your specific condition
- Monitor the success of previous treatments
Recent studies have shown that CO2 angiography is a safe and effective alternative to iodine contrast, particularly for patients with kidney problems. While image quality can be slightly lower with CO2, advancements in imaging technology are continually improving results.
Our practice carefully considers each patient’s needs when choosing between iodine and CO2 contrast. We aim to provide you with the most accurate diagnosis while prioritizing your safety and comfort. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We’re here to ensure you receive the best care for your vascular health.
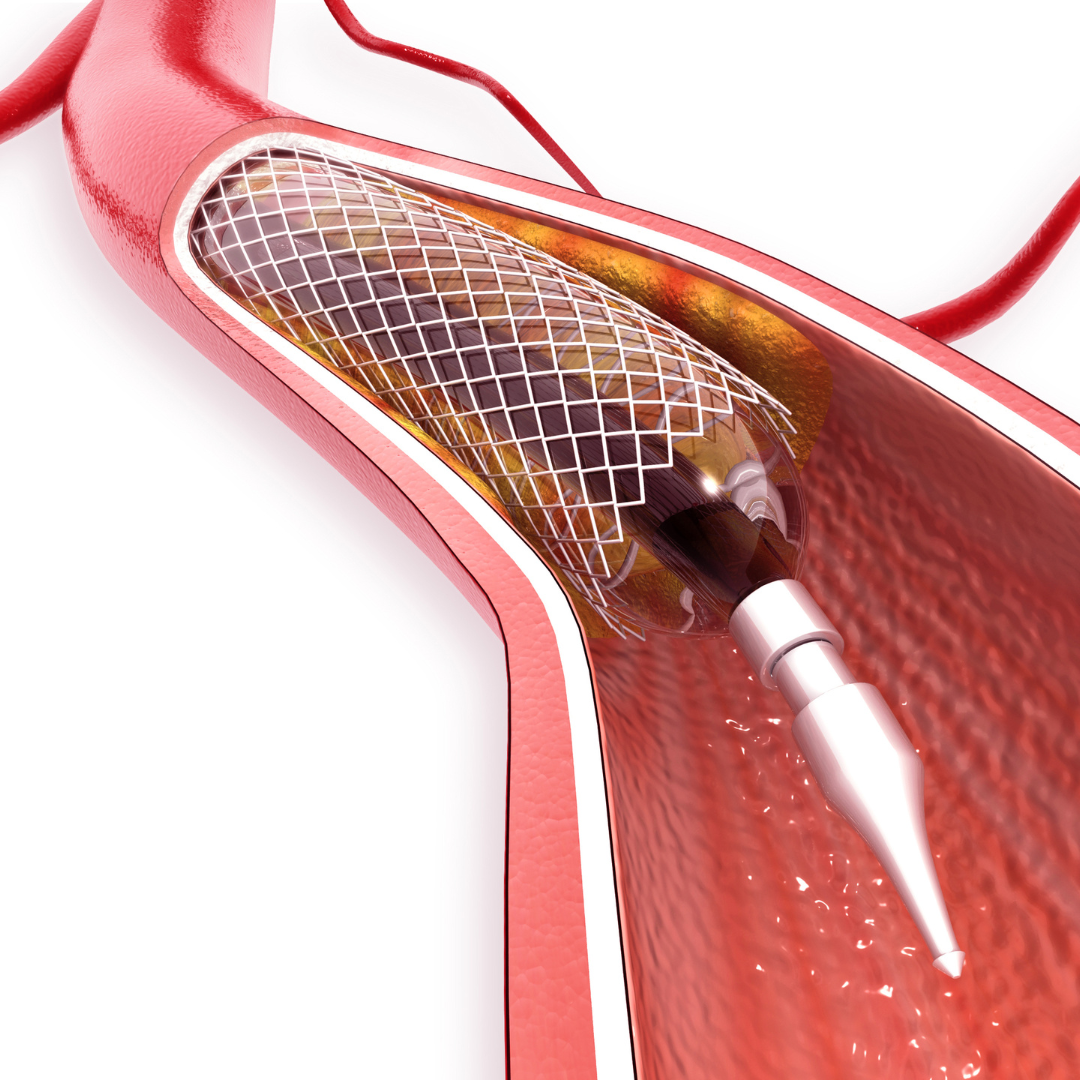
Lower Extremities Balloon Angioplasty: Restoring Blood Flow to Your Legs:
Balloon angioplasty is an important minimally invasive procedure that can significantly improve blood flow in the arteries of your legs. This treatment is particularly beneficial for those experiencing symptoms of peripheral artery disease (PAD), such as leg pain or cramping while walking.
Why is this procedure important?
Balloon angioplasty can:
- Restore blood flow to your legs and feet
- Reduce pain and discomfort when walking
- Improve your overall mobility and quality of life
- Help prevent more serious complications of PAD
What to expect during the procedure
The angioplasty process is straightforward and typically takes 1-2 hours:
- You’ll lie comfortably on an examination table.
- A small incision will be made, usually in your groin area.
- Your doctor will insert a thin tube (catheter) into an artery.
- Using X-ray guidance, the catheter will be threaded to the blocked area in your leg.
- A tiny balloon at the tip of the catheter will be inflated to push the plaque against the artery wall, widening the vessel.
- In some cases, a small mesh tube (stent) may be placed to help keep the artery open.
You’ll be awake during the procedure but receive medication to help you relax. Most people experience little to no discomfort.
Preparing for your angioplasty:
To ensure the best possible outcome:
- Inform your doctor of all medications you’re taking
- Follow any fasting instructions provided
- Arrange for someone to drive you home after the procedure
After the procedure
Most patients can go home the same day or the next morning. You’ll need to:
- Rest and limit activity for a few days
- Keep the incision site clean and dry
- Take prescribed medications as directed
- Attend follow-up appointments
Benefits to your health
Balloon angioplasty can significantly improve your quality of life by:
- Reducing leg pain and cramping
- Increasing walking distance without discomfort
- Improving circulation to promote the healing of leg wounds
- Potentially avoiding more invasive surgical procedures
Current guidelines from the Society for Vascular Surgery recommend considering balloon angioplasty for patients with lifestyle-limiting claudication who have not responded adequately to exercise therapy and medication. For patients with critical limb ischemia, balloon angioplasty is often the first-line treatment to restore blood flow and prevent limb loss.
At our practice, we’re committed to providing you with the best possible care for your vascular health. Balloon angioplasty is a safe and effective treatment that has helped many patients regain mobility and enjoy a better quality of life. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We’re here to support you every step of the way.
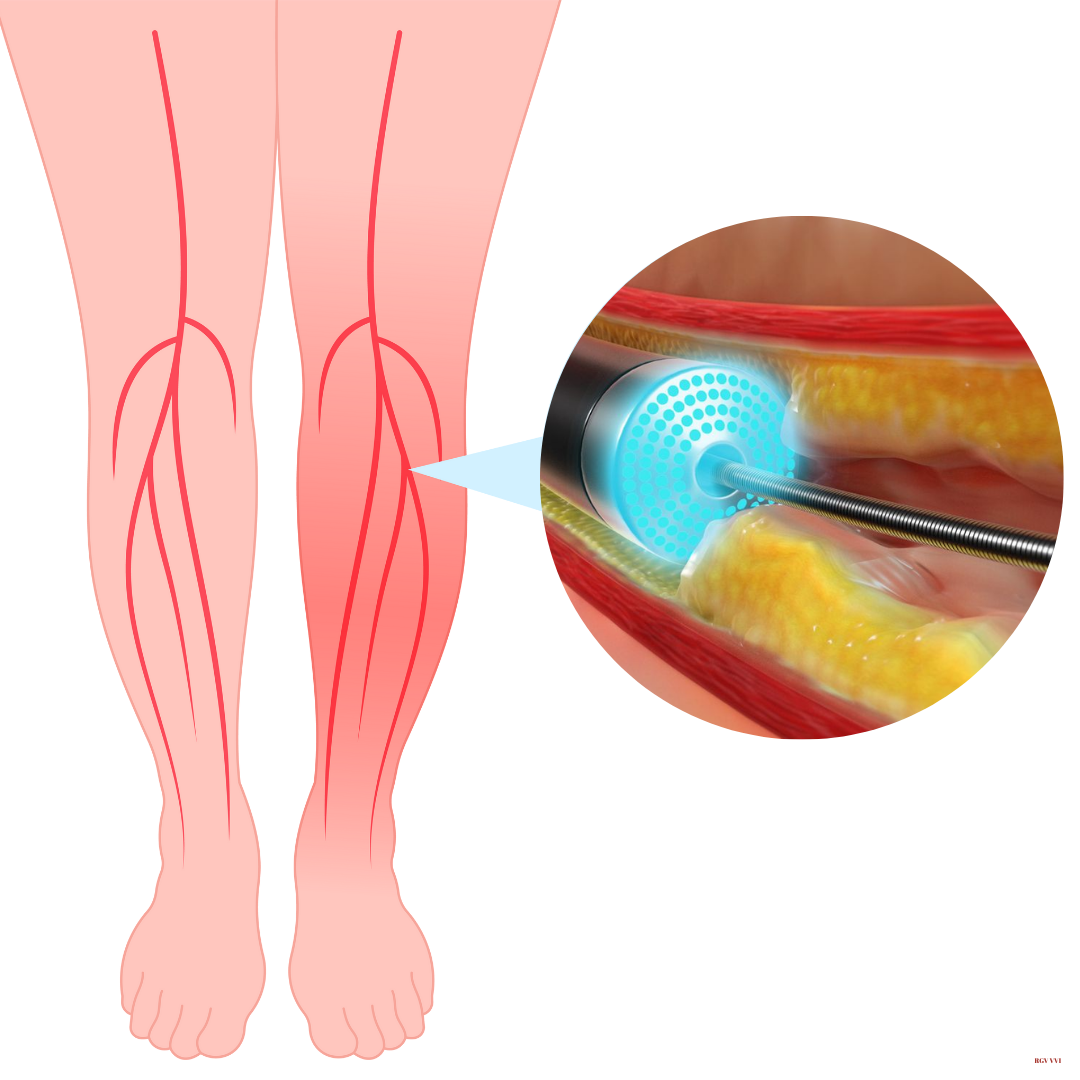
Lower Extremities Atherectomy: Laser and Orbital Options
Atherectomy is an advanced procedure for treating peripheral artery disease (PAD) in the legs. It’s a minimally invasive technique that removes plaque buildup from arteries, improving blood flow and reducing symptoms like leg pain and difficulty walking. Two effective types of atherectomy for the lower extremities are laser and orbital atherectomy.
Why is this procedure important?
PAD affects millions of people, particularly those over 40. When arteries in your legs become narrowed or blocked by plaque, it can lead to serious complications if left untreated. Atherectomy can:
- Restore blood flow to your legs and feet
- Reduce pain and cramping when walking
- Improve your mobility and quality of life
- Help prevent more serious issues like critical limb ischemia
Laser Atherectomy
This technique uses a catheter that emits high-energy light to vaporize plaque. It’s particularly effective for treating long, diffuse blockages and can help reopen arteries that have been previously treated with stents.
Orbital Atherectomy
This method uses a diamond-coated crown that orbits within the artery, sanding away plaque, especially calcified buildup. It’s highly effective for treating heavily calcified lesions that are challenging to treat with other methods.
What to expect during the procedure:
- You’ll lie comfortably on an examination table.
- Local anesthesia will be used to numb the area.
- Your doctor will make a small incision, usually in the groin area.
- A special catheter will be guided to the blocked area in your leg artery.
- The atherectomy device (laser or orbital) will remove the plaque.
- The procedure typically takes 1-2 hours.
You’ll be awake but sedated during the procedure, ensuring you’re comfortable.
Preparing for your atherectomy
- Inform your doctor of all medications you’re taking
- Follow any fasting instructions provided
- Arrange for someone to drive you home after the procedure
After the procedure:
- You’ll need to lie flat for a few hours to prevent bleeding
- Most patients can go home the same day or the next morning
- You should rest and limit activity for a few days
- Follow your doctor’s instructions on medication and wound care
- Attend all follow-up appointments
Benefits to your health
Atherectomy can significantly improve your quality of life by:
- Reducing leg pain and cramping
- Increasing how far you can walk without discomfort
- Improving circulation to help heal leg wounds
- Often avoiding the need for more invasive bypass surgery
Current guidelines from the Society for Vascular Surgery recommend considering atherectomy for patients with lifestyle-limiting claudication who haven’t responded adequately to exercise therapy and medication. For patients with critical limb ischemia, atherectomy can be a crucial treatment to restore blood flow and prevent limb loss.
Our practice carefully evaluates each patient to determine the most appropriate treatment. Laser and orbital atherectomy are safe and effective options that have helped many patients regain mobility and enjoy a better quality of life. If you have any questions or concerns about these procedures, please don’t hesitate to ask. We’re here to support you every step of the way to better vascular health.
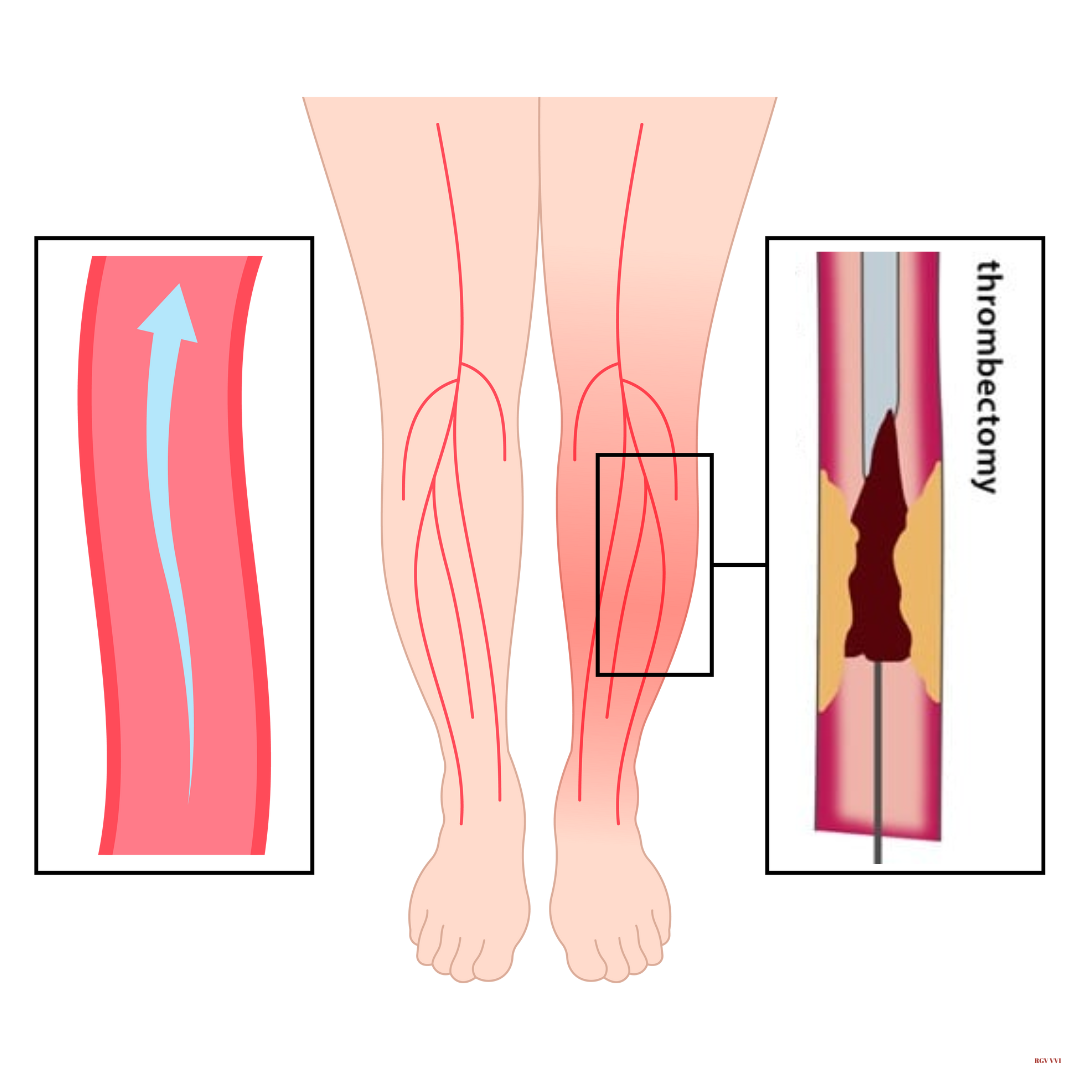
Lower Extremities Thrombectomy: Restoring Blood Flow to Your Legs
A lower extremities thrombectomy is an advanced, minimally invasive procedure used to remove blood clots from arteries in your legs. This treatment can quickly restore blood flow, relieve symptoms, and save limbs in severe blockages.
Why is this procedure important?
Blood clots in leg arteries can cause serious complications if left untreated. A thrombectomy can:
- Quickly restore blood flow to your legs and feet
- Relieve pain and swelling
- Prevent tissue damage and potential limb loss
- Improve your mobility and quality of life
What to expect during the procedure
The thrombectomy process is typically performed under local anesthesia and takes about 1-2 hours:
- You’ll lie comfortably on an examination table.
- A small incision will be made, usually in the groin area.
- Your doctor will guide a catheter to the clot in your leg artery.
- Special devices will be used to remove or break up the clot.
- Sometimes, a stent may be placed to keep the artery open.
You’ll be awake but sedated during the procedure, ensuring you’re comfortable.
Preparing for your thrombectomy:
- Inform your doctor of all medications you’re taking
- Follow any fasting instructions provided
- Arrange for someone to drive you home after the procedure
After the procedure
- You’ll need to lie flat for a few hours to prevent bleeding
- Most patients can go home the same day or the next morning
- You should rest and limit activity for a few days
- Follow your doctor’s instructions on medication and wound care
- Attend all follow-up appointments
Benefits to your health
A thrombectomy can significantly improve your condition by:
- Quickly relieving pain and swelling in your leg
- Restoring blood flow to prevent tissue damage
- Potentially saving your limb in severe cases
- Improving your ability to walk and perform daily activities
Current guidelines from vascular societies recommend considering thrombectomy for patients with acute limb ischemia, especially when there’s a risk of limb loss. It’s particularly effective when performed within 14 days of symptom onset.
Our practice carefully evaluates each patient to determine the most appropriate treatment. Thrombectomy is a safe and effective option that has helped many of our patients avoid serious complications and regain their mobility. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We’re here to support you every step of the way to better vascular health.
Lower Extremities Atherectomy
Lower Extremities Thrombectomy
Invasive Procedures for CVD
Sclerotherapy
Foam Sclerotherapy for Varicose Veins
Radiofrequency Ablation (RFA) for Venous
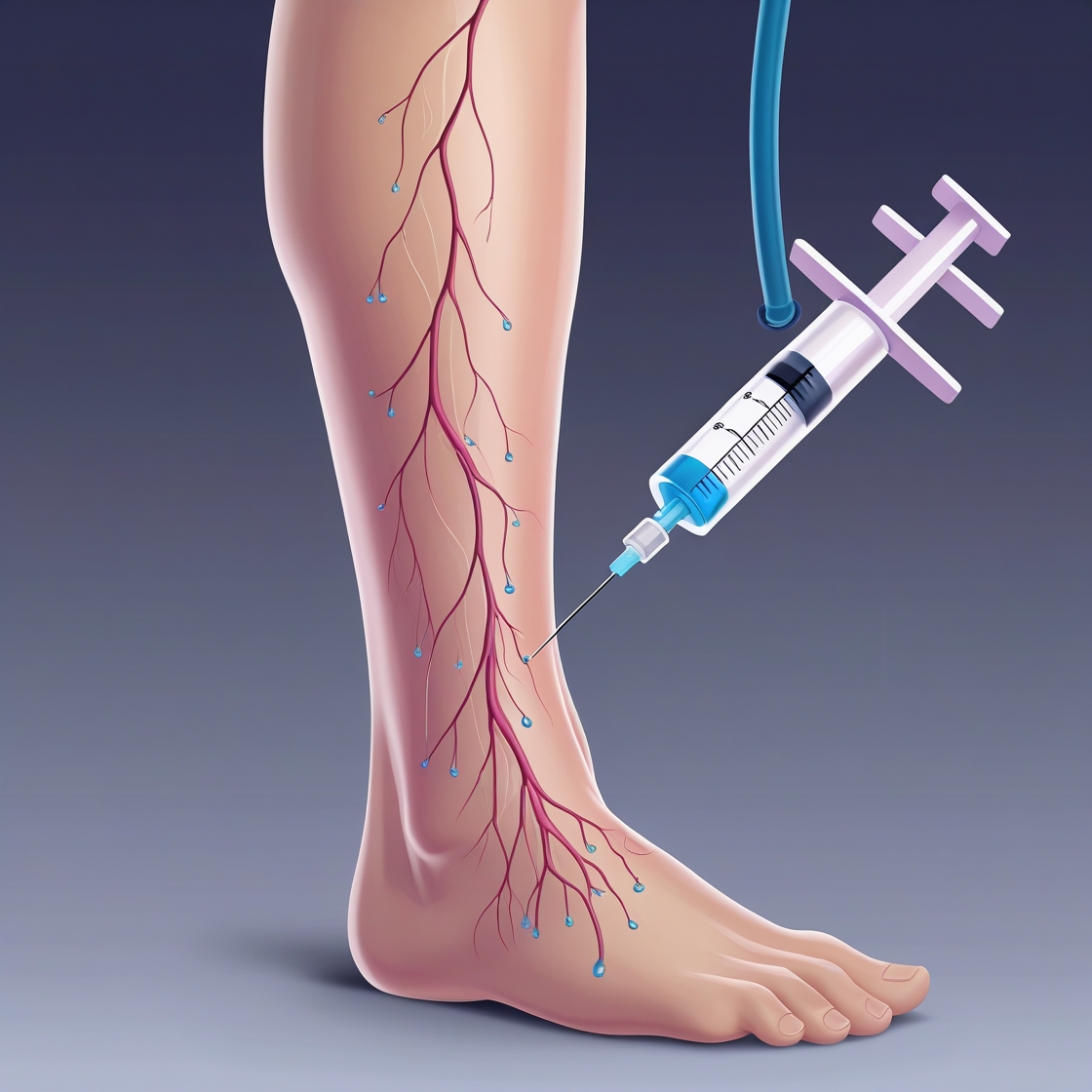
Sclerotherapy: Treating Spider and Reticular Veins
Sclerotherapy is a safe and effective treatment for spider and reticular veins, those small, unsightly blood vessels that can appear on your legs. This minimally invasive procedure uses injections to improve the appearance of your legs and relieve symptoms associated with these veins.
Why Consider Sclerotherapy?
Sclerotherapy can:
- Improve the appearance of your legs
- Reduce aching, burning, or swelling associated with spider and reticular veins
- Boost your confidence in wearing shorts or swimwear
Types of Sclerotherapy
We offer two types of sclerotherapy, tailored to the size of the veins being treated:
- Liquid Sclerotherapy for Spider Veins:
- It uses a special solution injected into the tiny spider veins
- This causes the veins to collapse and fade over time
- CO2 Sclerotherapy for Reticular Veins:
- It uses carbon dioxide mixed with the sclerosing solution
- It is more effective for slightly larger reticular veins
- It can treat veins that are harder to inject with liquid alone
What to Expect During the Procedure
Sclerotherapy is performed in our office and typically takes 30-60 minutes:
- You’ll lie comfortably on an examination table
- The treatment area will be cleaned
- Using a very fine needle, we’ll inject the solution into the targeted veins
- You may feel a slight burning sensation during injection, but it’s usually minimal
Preparing for Sclerotherapy
To ensure the best results:
- Avoid applying lotion to your legs on the day of treatment
- Wear loose, comfortable clothing
- Inform us of any medications or supplements you’re taking
After Your Treatment
- You can return to normal activities immediately
- Walking is encouraged to promote circulation
- Avoid strenuous exercise for a few days
- Wear compression stockings as directed (usually for 1-2 weeks)
- Avoid sun exposure to the treated areas for a few weeks
Results and Follow-up
While you may see some improvement immediately, the full effects of sclerotherapy develop over several weeks. For optimal results, most patients require 2-4 treatment sessions.
Is Sclerotherapy Right for You?
Sclerotherapy is an excellent option for many people, but it’s not suitable for everyone. During your consultation, we’ll assess your veins and medical history to determine whether this treatment is appropriate.
Current guidelines from the American Vein and Lymphatic Society support sclerotherapy as a first-line treatment for spider and small reticular veins. Studies have shown that sclerotherapy can effectively eliminate 50-80% of treated veins in a single session.
At our practice, we’re committed to helping you achieve healthier, more beautiful legs. If you have any questions about sclerotherapy or would like to schedule a consultation, please don’t hesitate to contact us. We’re here to provide you with the best possible care and results.
Foam Sclerotherapy for Varicose Veins: A Safe and Effective Treatment
Foam sclerotherapy is a minimally invasive procedure used to treat varicose veins. This treatment can significantly improve the appearance of your legs and relieve symptoms like pain, swelling, and heaviness.
Why is this procedure important?
Varicose veins are not just a cosmetic concern. They can cause discomfort and, if left untreated, may lead to more serious complications. Foam sclerotherapy offers several benefits:
- Minimally invasive with little to no downtime
- Effective in treating even large varicose veins
- It can be performed in an outpatient setting
- May prevent the progression of vein disease
What to expect during the procedure
- You’ll lie comfortably on an examination table.
- Your doctor will use ultrasound to guide the treatment.
- A small needle will be used to inject foam into the affected veins.
- The foam causes the vein walls to collapse and seal shut.
- The entire procedure usually takes 30-60 minutes.
Preparing for your treatment
- Wear loose, comfortable clothing
- Avoid applying lotions or perfumes to your legs
- Inform your doctor of all medications you’re taking
- Arrange for someone to drive you home after the procedure
After the procedure
- You’ll need to wear compression stockings for a few days to weeks
- Walking is encouraged, but avoid strenuous exercise for 1-2 weeks
- You may experience some bruising or discomfort, which is normal
- Follow-up appointments will be scheduled to monitor your progress
Current guidelines from vascular societies recommend foam sclerotherapy as an effective treatment option for varicose veins, particularly for recurrent varicose veins after surgery or for veins that are not suitable for other treatments.
Our practice carefully evaluates each patient to determine the most appropriate treatment. Foam sclerotherapy has helped many patients find relief from varicose veins and improve their quality of life. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We support you every step in your journey to healthier legs.
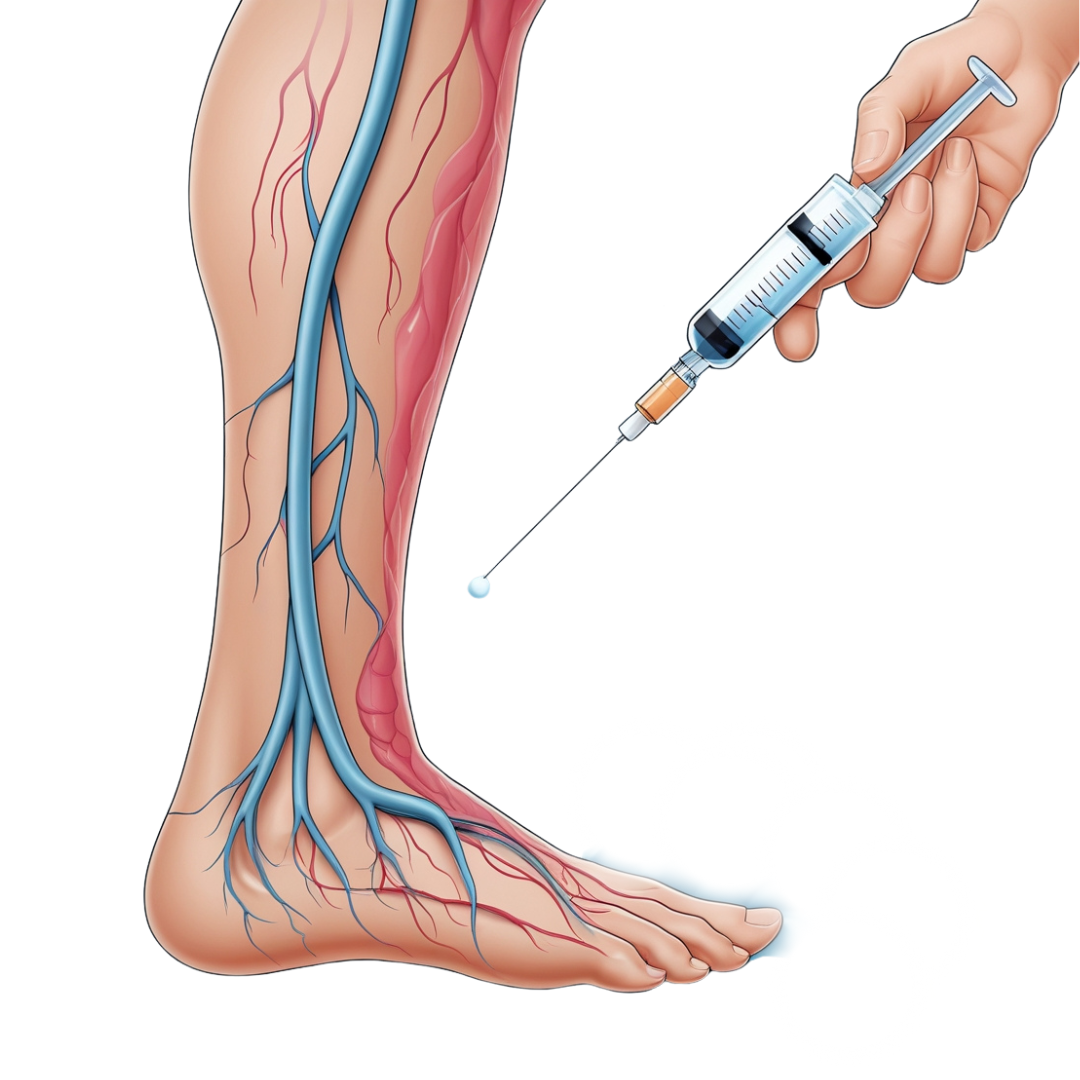
Chemical Ablation for Venous Insufficiency: A Safe and Effective Treatment
Chemical ablation is an innovative, minimally invasive procedure for treating venous insufficiency in the legs’ saphenous, perforator, and tributary veins. This treatment can significantly improve symptoms like leg pain, swelling, and varicose veins, enhancing your quality of life and overall health.
Why is this procedure important?
Venous insufficiency occurs when the valves in your leg veins don’t work properly, causing blood to pool in your legs. If left untreated, this condition can lead to serious complications like skin changes, ulcers, and even blood clots. Chemical ablation offers a safe and effective way to address these issues by closing off problematic veins, allowing blood to reroute to healthier veins.
What to expect during the procedure
- You’ll lie comfortably on an examination table.
- Your doctor will use ultrasound to locate the affected veins.
- A small needle will be used to inject a special foam medication (sclerosant) into the vein.
- The medication causes the vein walls to seal shut, eventually allowing the vein to be reabsorbed by your body.
- The entire procedure usually takes 30-60 minutes, depending on how many veins are treated.
You’ll be awake during the procedure, and most patients report minimal discomfort.
Preparing for your chemical ablation:
- Wear loose, comfortable clothing
- Avoid applying lotion to your legs on the day of treatment
- Eat normally and take your regular medications
- Bring compression stockings (your doctor will advise on the appropriate type)
After the procedure
- You can return to most normal activities immediately
- Wear compression stockings as directed by your doctor (usually for 1-2 weeks)
- Avoid strenuous exercise and hot baths for about a week
- Walk for at least 10 minutes daily to promote good circulation
- You may notice some mild bruising or hardness along the treated vein, which is normal and will resolve over time
Benefits to your health
Chemical ablation can significantly improve your symptoms and quality of life by:
- Reducing leg pain, swelling, and fatigue
- Improving the appearance of varicose veins
- Preventing more serious complications of venous insufficiency
- Offering a quick recovery with minimal downtime
Current guidelines from vascular societies recommend chemical ablation as a safe and effective option for treating venous insufficiency, particularly for patients who may not be suitable candidates for thermal ablation techniques.
Our practice is committed to providing you with the most appropriate and effective treatment for your venous health. Chemical ablation has helped many of our patients find relief from the discomfort and cosmetic concerns of venous insufficiency. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We’re here to support you every step of the way to better vascular health.
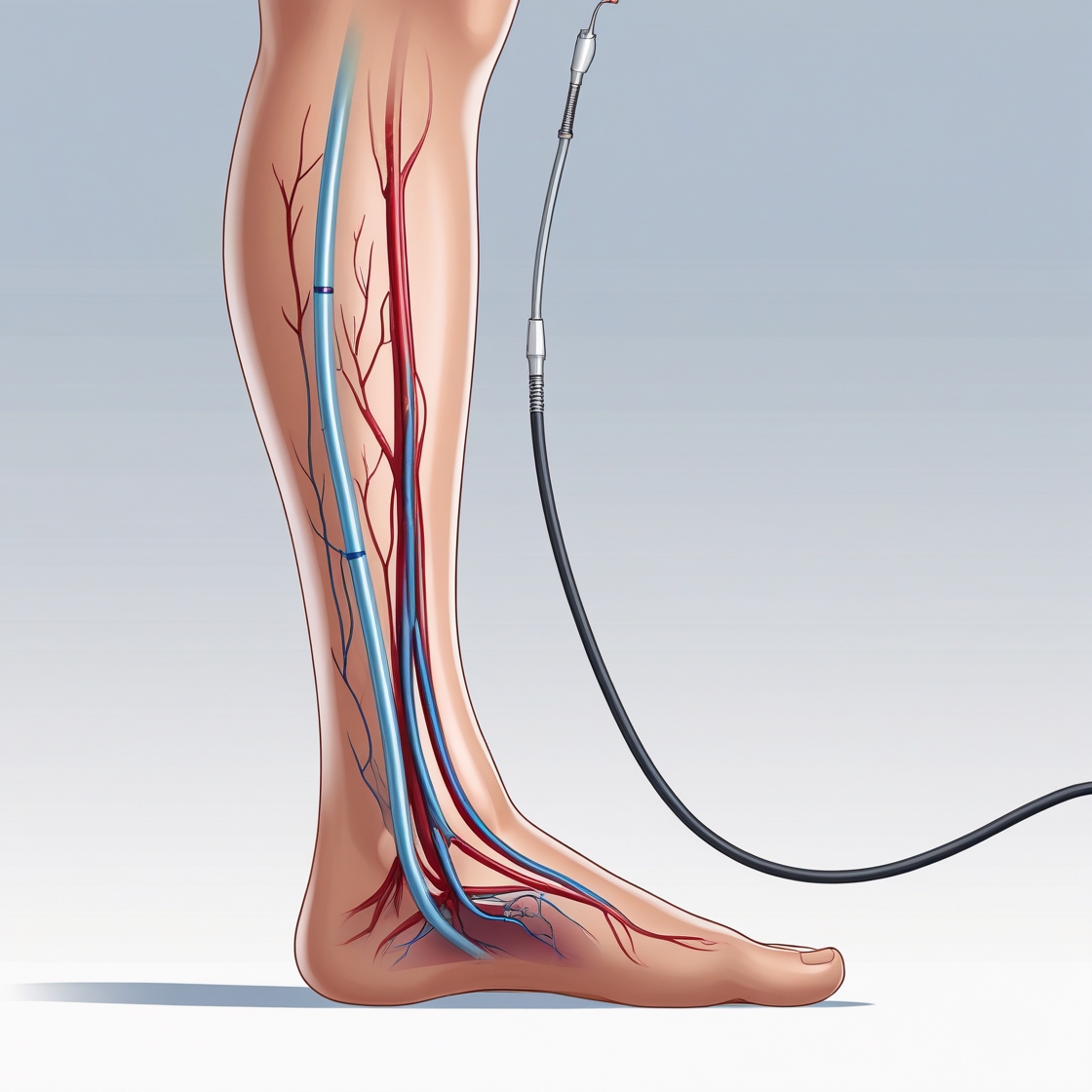
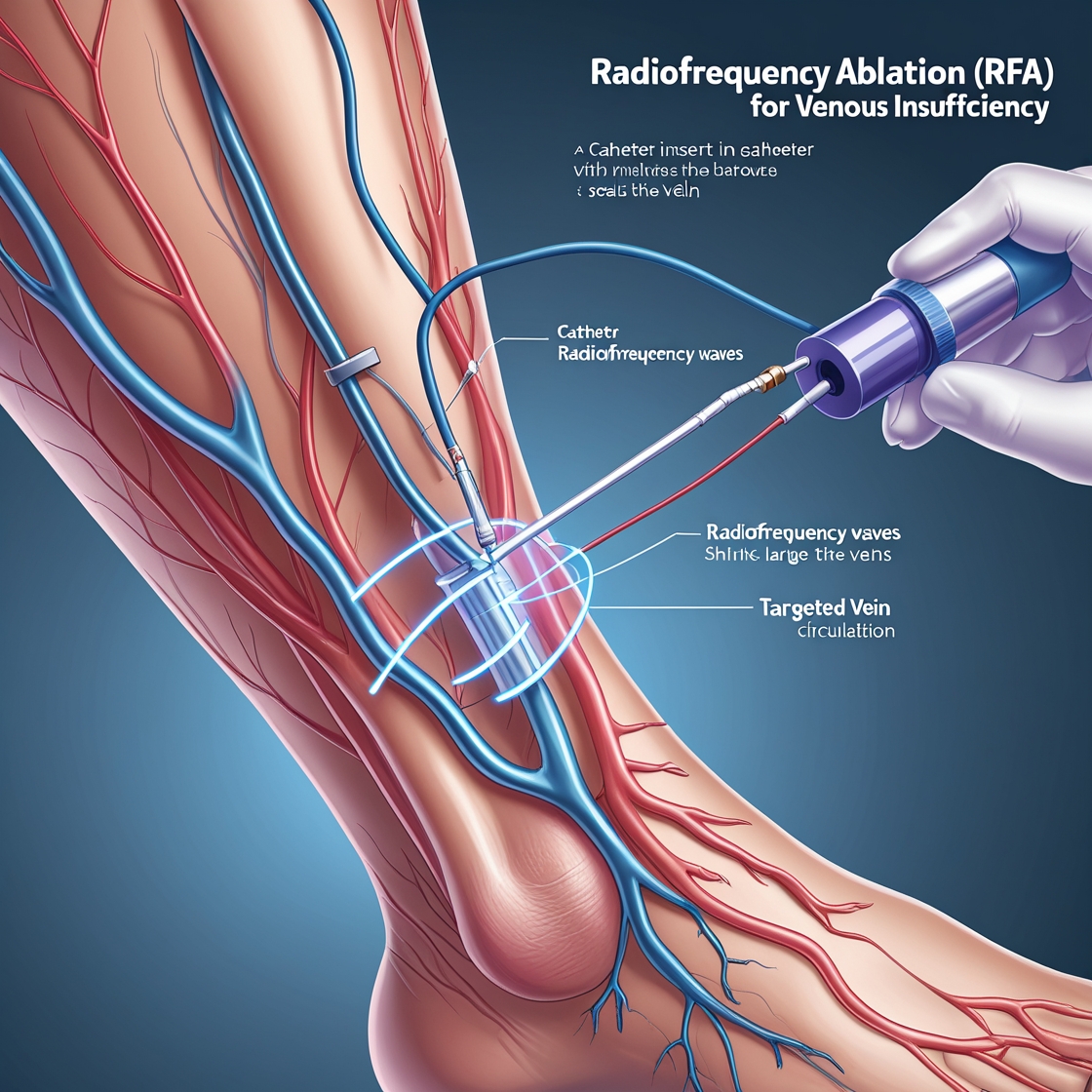
Radiofrequency Ablation (RFA) for Venous Insufficiency: A Modern Solution for Varicose Veins
Radiofrequency Ablation (RFA) of the saphenous vein is an innovative, minimally invasive procedure for treating venous insufficiency, a common condition that often leads to varicose veins. This treatment offers a quick, effective way to improve circulation in your legs and alleviate symptoms associated with varicose veins.
Why is this procedure important?
Venous insufficiency affects millions of people, causing symptoms like:
- Leg pain and heaviness
- Swelling
- Skin changes
- Varicose veins
Left untreated, it can lead to more serious complications. RFA can:
- Improve blood flow in your legs
- Reduce pain and swelling
- Enhance your leg appearance
- Boost your overall quality of life
What to expect during the procedure
RFA is typically performed in an outpatient setting and takes about 45-60 minutes:
- You’ll lie comfortably on an examination table.
- The treatment area will be numbed with local anesthesia.
- Guided by ultrasound, your doctor will insert a thin catheter into the affected vein.
- The catheter will deliver radiofrequency energy to heat and seal the vein.
- The catheter is then removed, and a compression bandage is applied.
You’ll be awake during the procedure, and most patients report little to no discomfort.
Preparing for your RFA:
- Avoid shaving your legs for 24 hours before the procedure
- Wear loose, comfortable clothing
- Arrange for someone to drive you home after the procedure
After the procedure
- You can usually return to normal activities the same day
- Wear compression stockings as directed by your doctor
- Walk regularly to promote healing
- Avoid strenuous exercise and heavy lifting for a week
- Attend follow-up appointments for ultrasound checks
Benefits to your health
RFA offers several advantages:
- High success rate in closing problematic veins
- Quick recovery with minimal downtime
- Improved leg appearance and comfort
- Long-lasting results
Current guidelines from the Society for Vascular Surgery and the American Venous Forum recommend RFA as a safe and effective treatment for symptomatic varicose veins caused by saphenous vein reflux. Studies have shown that RFA has a 95% success rate in closing treated veins, with results lasting up to 5 years or more.
Our practice is committed to providing you with the most advanced and effective treatments for venous insufficiency. RFA has helped many patients find relief from varicose veins and improve their leg health. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We’re here to support your journey to healthier, more comfortable legs.
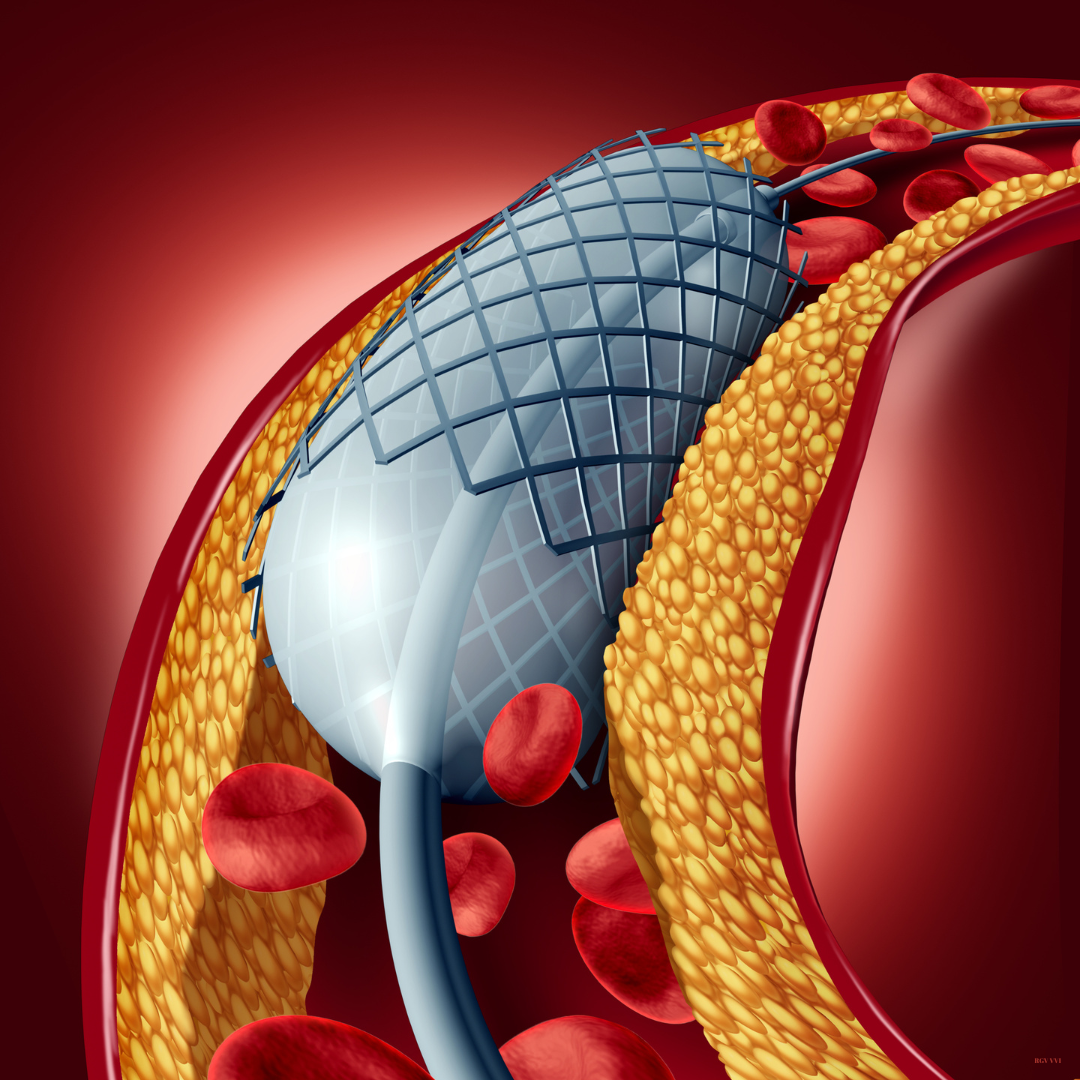
Venous Stenting in Iliac Vein Compression: Restoring Healthy Blood Flow
Iliac vein compression, sometimes called May-Thurner syndrome, occurs when the iliac artery presses on the iliac vein in your pelvis, restricting blood flow from your legs back to your heart. This can lead to leg pain, swelling, and even blood clots. Venous stenting is a minimally invasive procedure that can effectively treat this condition and improve your quality of life.
Why is this procedure important?
Venous stenting can:
- Relieve leg pain and swelling
- Reduce your risk of developing blood clots
- Improve your overall circulation
- Help heal venous ulcers if present
- Enhance your mobility and quality of life
What to expect during the procedure
Venous stenting is typically performed under local anesthesia and mild sedation. Here’s what you can expect:
- You’ll lie comfortably on an examination table.
- A small incision will be made, usually in your groin area.
- Using X-ray guidance, your doctor will thread a catheter to the compressed vein.
- A balloon may be inflated to widen the vein.
- A stent (a small mesh tube) will be placed to keep the vein open.
- The procedure usually takes about 1-2 hours.
Preparing for your procedure
- Inform your doctor of all medications you’re taking
- Follow any fasting instructions provided
- Arrange for someone to drive you home afterward
After the procedure
- You’ll need to lie flat for a few hours to prevent bleeding
- Most patients can go home on the same day
- You should rest and limit activity for a few days
- Follow your doctor’s instructions on medication and wound care
- Attend all follow-up appointments
Benefits to your health
Current guidelines from vascular societies recommend considering venous stenting for patients with significant symptoms who haven’t responded adequately to conservative treatments. Studies have shown that venous stenting can provide significant relief, with one review reporting symptom improvement in 87% of patients and ulcer healing in 56% of cases.
Our practice carefully evaluates each patient to determine the most appropriate treatment. Venous stenting is a safe and effective option that has helped many patients regain mobility and enjoy a better quality of life. If you have any questions or concerns about this procedure, please don’t hesitate to ask. We’re here to support you every step of the way to better vascular health.
Venoplasty (Balloon/Stent): A Minimally Invasive Treatment for Vascular Blockages
Venoplasty is a minimally invasive procedure used to treat vascular blockages in the veins. By using a balloon or stent to open narrowed or obstructed veins, this procedure improves blood flow, helping to alleviate symptoms related to poor circulation and enhance overall vascular health.
Why is this procedure important?
Venous blockages can lead to a variety of complications, including:
- Swelling in the legs or arms
- Leg pain or heaviness
- Skin changes
- Ulceration or other chronic conditions
Left untreated, these issues can worsen and negatively impact your quality of life. Venoplasty can:
- Restore normal blood flow
- Reduce swelling and discomfort
- Prevent further complications
- Enhance your overall vascular health
What to expect during the procedure
Venoplasty is typically performed as an outpatient procedure and usually takes about 30-90 minutes:
- You’ll be positioned comfortably on an examination table.
- Local anesthesia will be applied to numb the treatment area.
- Using ultrasound guidance, a thin catheter will be inserted into the affected vein.
- A balloon attached to the catheter will be inflated to widen the vein, and in some cases, a stent may be placed to keep the vein open.
- Once the procedure is complete, the catheter is removed, and a compression bandage is applied.
You will remain awake during the procedure, and most patients experience minimal discomfort.
Preparing for your venoplasty
- Avoid eating or drinking for a few hours before the procedure (as directed by your doctor).
- Inform your doctor of any medications you are currently taking.
- Wear loose, comfortable clothing on the day of the procedure.
- Arrange for someone to drive you home afterward.
After the procedure
- You may resume most normal activities within 24 hours.
- Wear compression stockings if recommended by your doctor.
- Walk regularly to support blood flow and healing.
- Avoid strenuous activities for at least a week.
● Attend follow-up appointments to ensure the procedure’s success.
Benefits to your health
Venoplasty offers several benefits, including:
- Improved circulation and reduced symptoms
- Minimal recovery time and a quick return to normal activities
- A safe and effective alternative to more invasive procedures
- Long-term improvement in your vascular health
Current guidelines from vascular societies recommend venoplasty for patients experiencing significant symptoms due to venous blockages that have not responded to conservative treatments. Research shows that balloon angioplasty and venous stenting can provide substantial relief, with studies indicating symptom improvement in a large percentage of patients and long-term vein patency rates of over 80%.
At our practice, we carefully assess each patient to ensure the most suitable treatment approach. Venoplasty is a safe, effective option that has helped many individuals improve circulation, reduce symptoms, and enhance their quality of life. If you have any questions or concerns about the procedure, please feel free to reach out. We are committed to supporting you on your journey to better vascular health.
Venous Stenting in Iliac Vein Compression